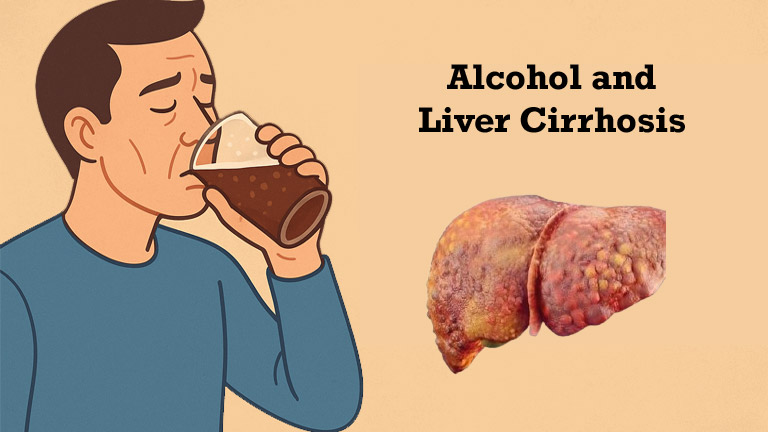
Did you know that excessive alcohol consumption leads to millions of deaths worldwide? In 2023, alcohol was a factor in over 50% of the 56,975 cirrhosis deaths worldwide. Approximately 1.26 million people died from liver cirrhosis and other liver diseases in 2019. This is why alcohol is considered a major cause. Interestingly, alcohol sales have increased by up to 54% in many countries during the COVID-19 pandemic. Given these facts, it is important to understand the risk of developing liver cirrhosis in people who drink alcohol and what precautions we should take.
What is Liver Cirrhosis?
Liver cirrhosis is a serious liver condition in which normal liver cells are damaged and replaced by scar tissue. This photo shows white scar tissue replacing red tissue on the surface of a cirrhotic liver. This condition disrupts the liver’s vital functions, such as processing nutrients, balancing hormones, and neutralizing toxins. Although early-stage fatty liver can be cured by quitting alcohol, the scarring that develops during cirrhosis becomes permanent. Unfortunately, once cirrhosis develops, it cannot be completely cured. Therefore, prevention is the best approach. Earlier, you may feel weakness, develop fatty liver, or notice fluid buildup in the abdomen along with swelling in your hands and feet. If it is detected at an early stage and you stop drinking, your lifespan can increase.
Effects of Alcohol on the Liver
Heavy drinking can be very harmful to the liver. In fact, excessive alcohol consumption is the most common cause of liver cirrhosis. In the first stage, alcohol causes fatty liver (fat deposits) in the liver, as almost all heavy drinkers develop fatty liver. Continued heavy drinking can lead to liver inflammation (alcoholic hepatitis), which occurs in about one-third of people. Eventually, scar tissue forms, leading to liver cirrhosis. According to the Mayo Clinic, after 10 years or more of continuous heavy drinking, approximately 10-20% of people develop cirrhosis. The liver has the ability to withstand injury and heal, but continued alcohol consumption weakens this ability. The Mayo Clinic states that fatty liver can resolve within a few weeks of quitting alcohol, but the scars of cirrhosis are permanent.
Microscopic View of Cirrhosis
This is a microscopic view of liver tissue damaged by cirrhosis, showing white, scarred tissue surrounded by red, healthy tissue. During cirrhosis, scarred (fibrotic) tissue forms in many areas of the liver, slowing down the liver’s normal function. According to the Mayo Clinic, approximately 100% of heavy drinkers have fatty liver, and 10–20% have cirrhosis. The image clearly shows that in cirrhosis, healthy cells are replaced by fibrotic tissue, which impairs liver function.
Risks for Alcoholics
You may be relieved to know that not every alcoholic develops cirrhosis. Several studies have found that the rate of developing cirrhosis in heavy drinkers is approximately 10–20%. The Mayo Clinic and other research confirm this figure. This means that many people avoid cirrhosis despite heavy drinking. Research has also found that most people with alcoholic cirrhosis consume 30–50 grams or more of alcohol per day. This may also depend on genetic factors or other underlying conditions. For example, women may have a higher risk of cirrhosis than men with the same amount of alcohol. Furthermore, other conditions, such as obesity and diabetes, can also increase the risk.
Risk Factors
Long-term heavy drinking puts significant strain on the liver. Experts consider heavy drinking to be 5 or more standard drinks (about 70/55 grams of alcohol) per day for men and 4 or more for women. Drinking consistently for such a long period of time significantly increases the risk of cirrhosis.
- Alcohol affects women more quickly. Studies show that women have a higher risk of cirrhosis than men with the same amount of alcohol.
- Some genetic traits may alter risk. Research has shown that people with certain gene variants may be less likely to develop cirrhosis even after heavy drinking.
- Other health conditions are also important. Conditions such as diabetes, obesity, or high blood pressure put additional strain on the liver. In such cases, the risk of cirrhosis increases by 2.4 times in heavy drinkers.
Prevention and Precautions
You have to stay under the supervision of a hepatologist who can recommend that you stop drinking and liver and other body tests every 3 or 6 months.
- Limit alcohol consumption: It is considered safe for healthy men to limit their daily intake to two standard drinks and for women to one. Drinking more than this can increase liver strain.
- Drinking with food is beneficial: Consuming alcohol with food slows its absorption in the body. Research has found that drinking alcohol with food may reduce the risk of cirrhosis, while frequent drinking on an empty stomach doubles the risk.
- Lead a balanced lifestyle: Eat adequate nutrients, exercise regularly, and maintain weight control. Conditions like obesity and diabetes increase the risk of liver disease.
- Get regular checkups: If you’ve been drinking alcohol for a long time, consult a doctor regularly and have your liver checked. Cirrhosis doesn’t cause any obvious symptoms in the beginning, so testing is crucial for early detection.
- Seek help when needed: If your alcohol consumption isn’t under control, don’t hesitate to seek help from a counselor or helpline. You can get rid of alcohol with the treatment services available in Oregon.
Keep in mind that once cirrhosis develops, it can lead to life-threatening complications – conditions like fluid retention, bleeding, and confusion. Ultimately, the most effective way to prevent liver cirrhosis is to control your alcohol intake. Taking care of your liver is your responsibility. Make wise decisions and take care of your health.